This July, Deft Research will publish a new consumer survey report devoted to consumers’ use and experience with Digital Health Technology. In anticipation of the July report, the analysis below explores digital health technology using data from a 2019 survey.
Introduction
In observing the current COVID-19 crisis, many people are coming to believe that telemedicine’s time has come. Under circumstances of high contagion and imminently overwhelmed resources, previous inhibitors to telemedicine’s adoption – regulation, reimbursement, consumer and provider acceptance — have wilted.
Forward-looking organizations speculate that on the other side of this crisis, telemedicine will have become widely used and consumers will have developed a liking for it. At that point, we may see the health system changed forever.
Strategy during Crisis
This is a terrible time for strategic purchases. The COVID-19 situation has compelled organizations to adopt telemedicine and other digital technology solutions immediately. But this leaves unaddressed concerns about the wisdom of investments and returns over time.
When new circumstances arise, previous survey research may help reduce uncertainty. Below, findings illuminate how health threats and lack of health care access influence consumer use of digital health technology. This leads to discovery of the relationships between personal health, access to care, and digital health technology. Where investments may have been made in uncertainty, information such as this, can reduce the uncertainty of how the investment will be used going forward.
We asked respondents whether they had received a new diagnosis in the past year, and a series of questions about digital health technology use.
Visits to health information websites are more common among those with a new diagnosis.
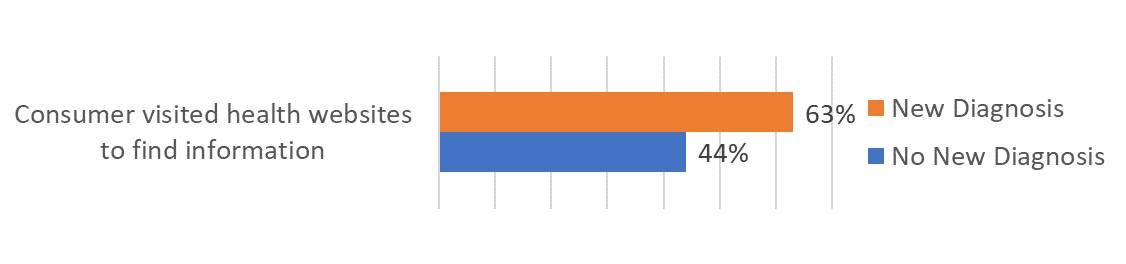
From this finding we see that consumers with a new diagnosis were more likely to seek information from websites. Urgency and convenience are probably factors in taking this course to learn more.
Newly diagnosed patients are more willing to install apps. Telehealth
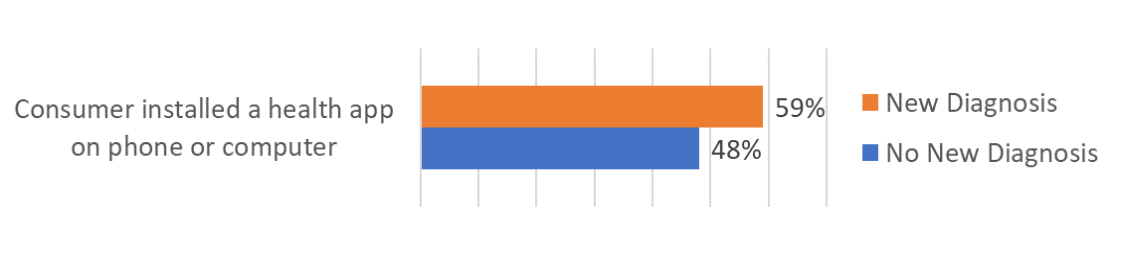
This finding shows that newly diagnosed patients are more frequently willing to commit their devices to health information and services.
Newly diagnosed patients are more likely to be heavy users of account-based services.
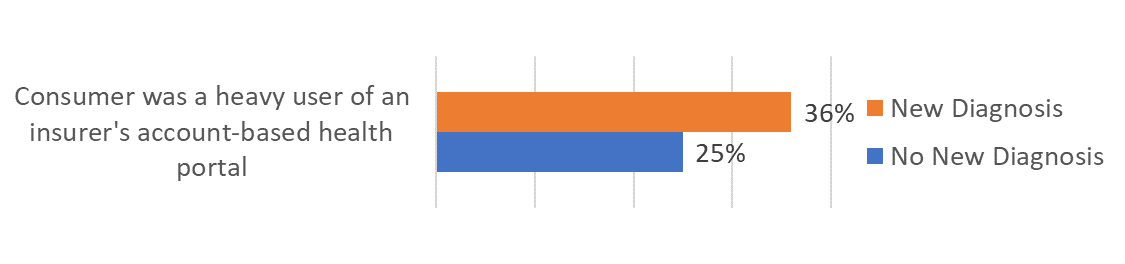
By “account-based” we mean a digital service that requires the user to register by providing personal information and establishing a username and password. The result above indicates newly diagnosed persons are more willing to do this, which means they are more willing to be personally identified, and to signal they want to have a more personalized relationship.
Newly diagnosed patients are more likely to use online chat in a health care context.
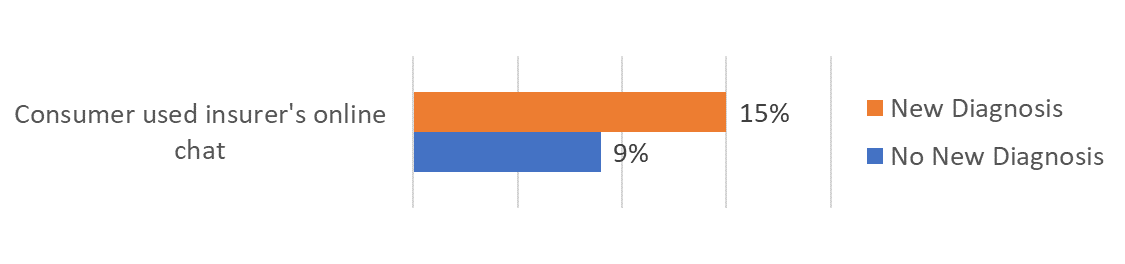
The frequency of using online chat falls behind other forms of digital health technology use. But telemedicine does not need to be limited to video conferencing. Chat is a path toward efficiency while meeting consumer needs for real-time response.
Access to health care also influences the use of technology. Our survey captured the insurance status of our respondents. This created a classification based on the source of insurance: an ACA plan, Medicaid, or no insurance. Our past consumer studies have shown that not having any insurance corresponds to having less health care access (see Deft’s consumer shopping and switching, and member experience studies).
When they have received a new diagnosis, persons with no insurance increase their use of health websites more than persons with insurance.
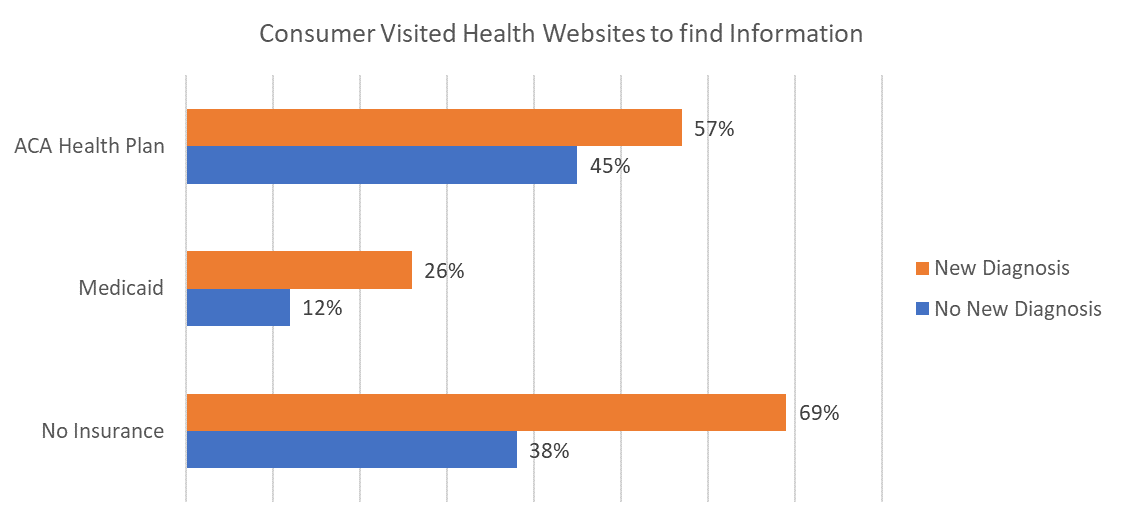
In the absence of insurance coverage uninsured persons rely more on available websites for information. Past studies have shown that persons with no insurance are less likely to regularly visit the doctor and to have a primary care relationship. In the absence of access, digital technology may be used to fill the gap.
Compared to insured persons, newly diagnosed persons with no insurance are more likely to have installed apps.
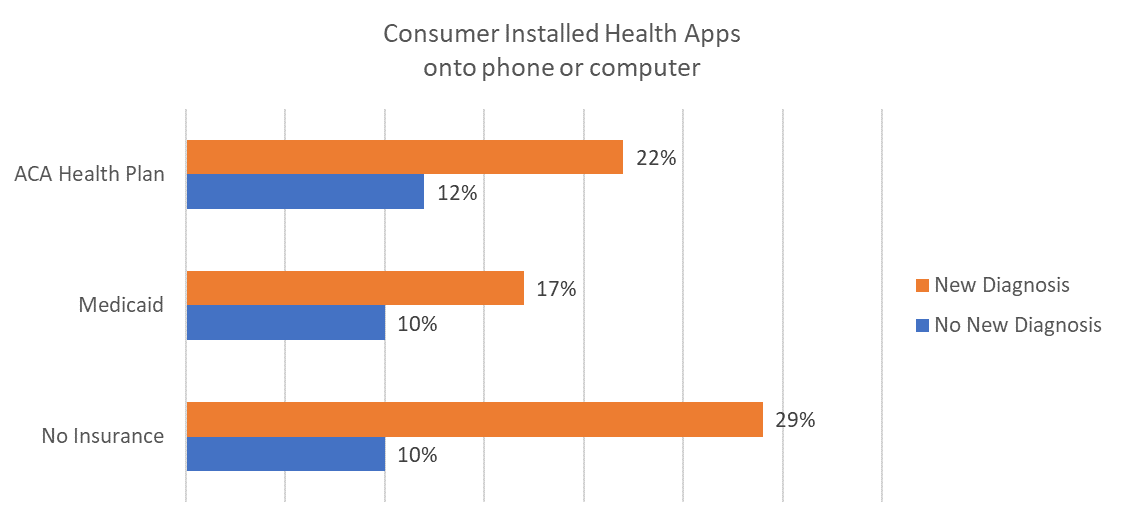
In the absence of health care relationships, uninsured persons may turn to digital health technology for support.
A new diagnosis is a threat to patients receiving it. Today, for all people, COVID-19 creates a similar threat experience. Observing rates of digital health technology use, we see that those with a new diagnosis (threat) have increased acceptance of the tech, and willingness to commit their devices to it.
Through the lens of consumer acceptance we have seen that a substantial portion of care delivered could occur through digital channels. The data above shows that digital channels would improve access to care for those with new health conditions.
Persons with no health insurance, are more likely than insured persons to use technology when they receive a new diagnosis. The findings connect lack of insurance and lower care access to increased use of digital health technology. The use of technology will have consequences: for example, it may be used to fill gaps in knowledge, dubious and not, and it may be used to assess whether to risk financial loss by incurring an appointment’s copayment. In the case of the uninsured, it is likely that advice and recommendations gained through digital channels come from sources lying outside of the medical establishment. The uninsured population has been growing in the past two years. Providing accurate, reliable digital resources so that members of the public have a better chance of obtaining better guidance, seems more important than ever.